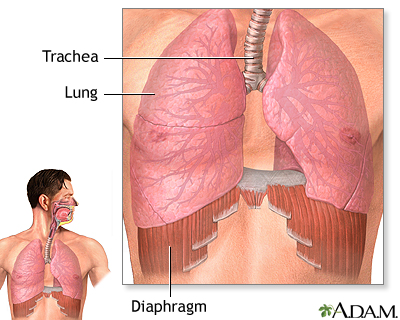
Unless you have lung disease. Well, you still need the oxygen, but you simply can't get it. When breathing becomes sufficiently difficult that your life is endangered, you'll be lucky to get on an organ donor list, and wait until someone dies who is a match to you. More often than not, you'll die before you get that transplant.
The lucky ones will benefit from another organ donor's loss of life and get a chance to live their own but breathing will come with its own costs if the organ isn't rejected, then expecta lifetime of anti-rejection drugs, and persistent, constant medical followup. At best.What if that wasn't necessary, but we could grow our own lung replacements? No long list-wait, no rejection drugs" just a nice new set of lungs made especially for us? Lab engineered lungs that let us have better lungs than we were born with!
That's exactly what two different researchers are working towards, and their endeavors are featured in The Scientist, June 24, in New lab-grown lungs.
Bioengineer and vascular biologist Laura Niklason of Yale University and her colleagues may have developed a way to eventually address these issues.
But wait - there's more! Barely over onehundred miles away, researchers at Harvard's Wyss Institute for Biologically Inspired Engineering have developed the "lung on a chip'. Not for implantation, but for additional research the chip can be used as an in vitro model for testing drugs and toxic effects of any variety of substances without using animals. Besides the obvious benefit to animals, there are other advantages of such a system, one of the most appealing is the speed at which new drugs can be tested is considerably faster if we're not waiting on the animals to be prepared for testing.Treating adult rat lungs with detergent solutions to remove their cellular components gave the researchers their starting point -- a lung skeleton, or the extracellular matrix that gives the lungs their structure. The team then repopulated the lungs with epithelial and endothelial cells from rat lungs, which grew over the scaffolds to create brand new lungs.
The researchers then implanted the new lungs into rats for up to two hours, during which time they found evidence that the engineered lungs were successfully participating in gas exchange. However, they also started to see some blood clots form in the vasculature of the lungs, as well as small amounts of leakage of blood into the airways, which most likely stemmed from an imperfect matrix and incomplete covering of new cells, Niklason (shownat right)said.
"Clearly we're close, but not all the way there yet," she said. "We really view this work as laying a scientific and technological basis for regenerating lungs in the long term."
Still, Macchiarini said, this is an important step. "The door is open now in the sense that we now have the tools to investigate how tissue engineering can generate lungs."
The end goal, which may still be a couple of decades away, Niklason said, is to use a patient's own cells to build an implantable lung, eliminating the potential rejection problems that come along with organ transplantation. This procedure would also broaden the potential pool of scaffold donors to include cadaveric organ donors and even large animals, she added.
The chip is constructed of a porous, flexible polymer, on which human epithelial and endothelial cells are cultured, much like Niklason's engineered rat lungs. The cells are then subjected to a lung-like environment, both in terms of their exposure to air on one side and fluid on the other, as well as the mechanical stretching that results from normal breathing, "recapitulating organ-level function" on a small, manageable chip, cell biologist Don Ingber said.
Plus, because the polymers on which the lung cells are cultured are clear, Ingber (shown at right) added, it is possible to do high resolution imaging of the tissue's interactions with the drug or toxin being tested, as opposed to in an animal, where "it's really hard to see what's going on."
"You had everything that you would in vivo except that here you have it externally," said tissue engineer and anesthesiologist Joaquin Cortiella of the University of Texas Medical Branch in Galveston, who did not participate in either study. "It's a way to test anything from pathogens to toxic things to drug studies."
"This paper [is] a major advance for evaluating toxicological methods, [as well as] pharmacological studies [and] nanomedicine," agreed Macchiarini. However, he added, it will not replace animal studies altogether. "In your body, you have thousands of reactions at once. We need to take into account."
(Note: You can view every article as one long page if you sign up as an Advocate Member, or higher).